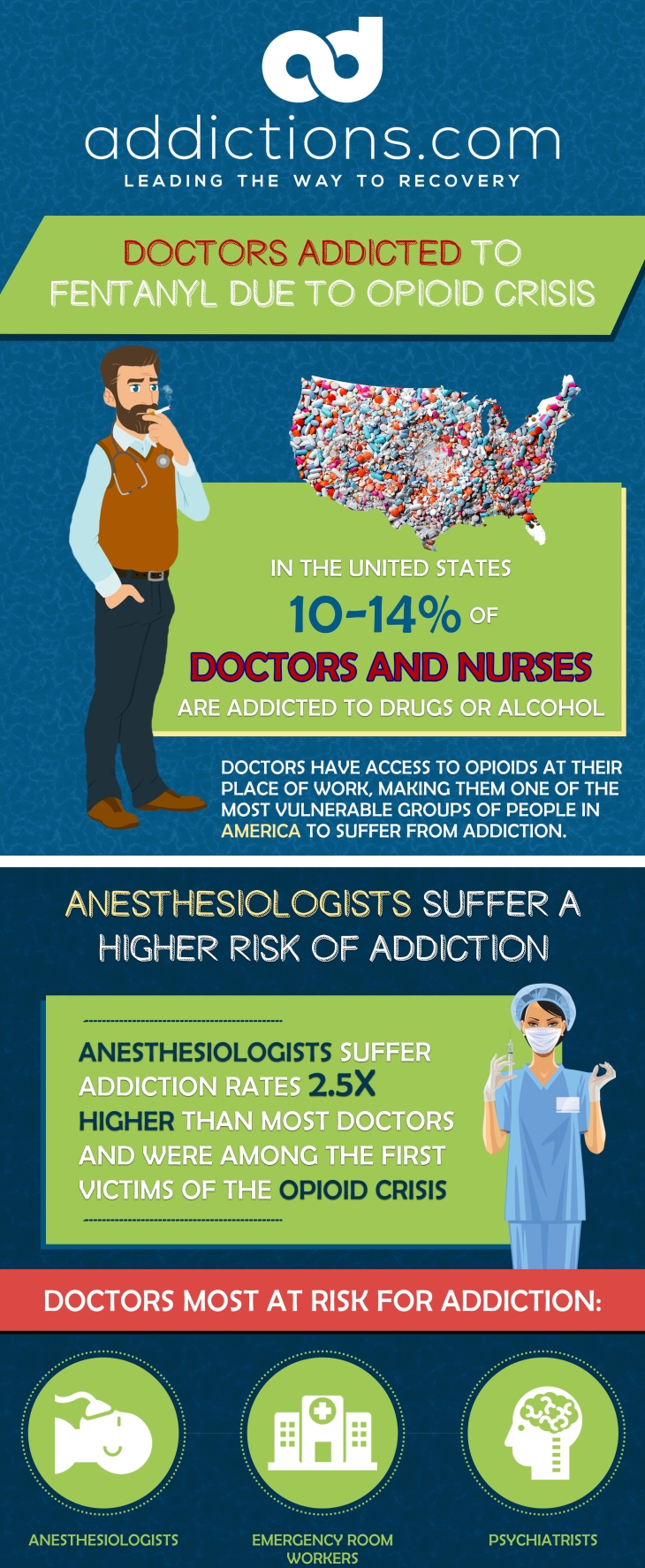
It’s unsettling to think about the concept of doctors fighting substance use disorders. In the United States, an estimated 10 to 14 percent of nurses and physicians are addicted to drugs or alcohol. While doctors may be considered some of our greatest heroes, it’s important to remember that doctors are only human like the rest of us, and aren’t invincible when it comes to addiction.
When compared to physicians in other medical specialties, anesthesiologists are most susceptible to drug use disorders, followed by emergency room workers and psychiatrists. A five-year study shows that anesthesiologists suffer addiction rates that are 2.5 times higher than those of other U.S. doctors. Anesthesiologists have increased access to drug supply, and can easily divert drugs for personal use without anyone noticing. These doctors also spend lots of time in fast-paced, high-stress work environments, which further contribute to their problems with addiction.
In tandem with America’s current opioid crisis, fentanyl abuse is on the rise among doctors in anesthesiology. Reports from addiction treatment centers show that fentanyl is the most commonly abused substance among anesthesiologists. Fentanyl is also one of the leading drivers behind opioid overdoses in the U.S., and can result in death with just one use.
Here’s a close look at the link between anesthesiology and fentanyl abuse, along with addiction treatments recommended for those who practice this medical specialty.
Why are Anesthesiologists Susceptible to Drug Use Disorders?
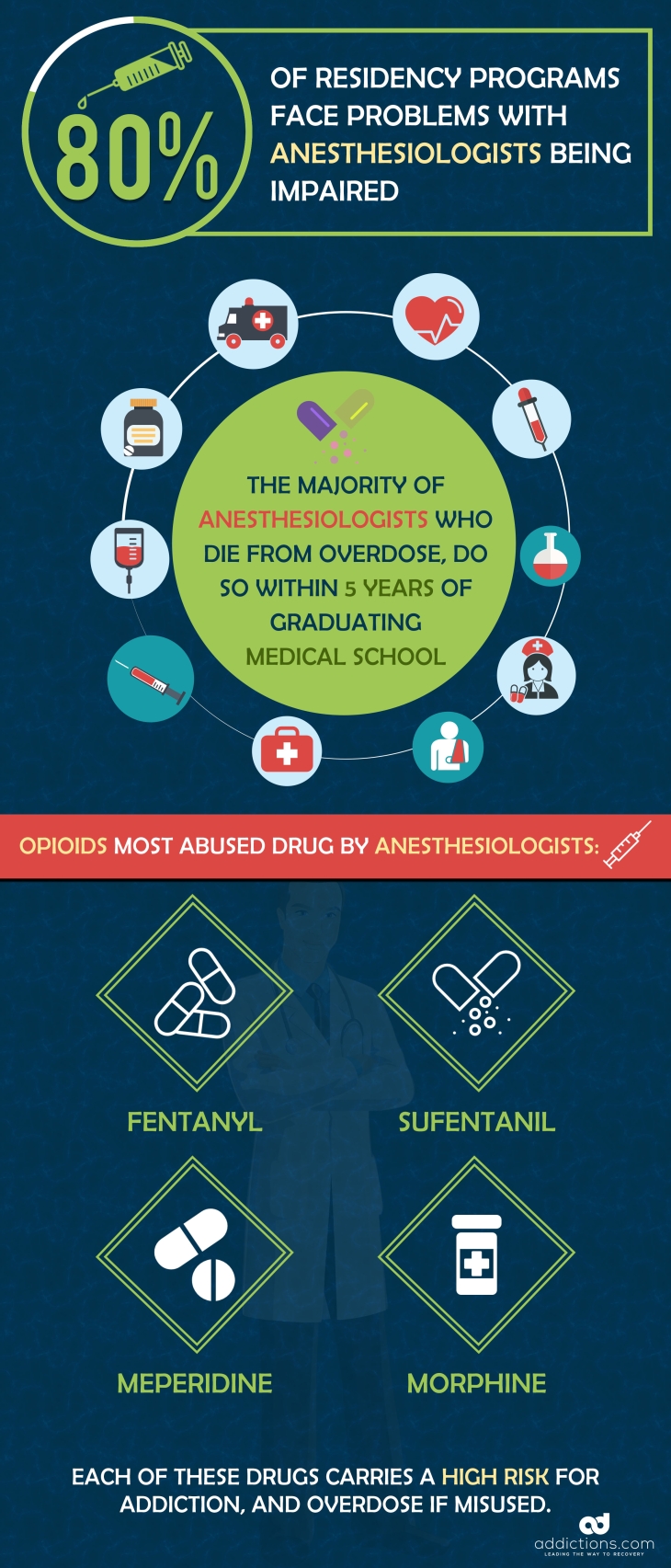
Anesthesiologists are surrounded by large amounts of drugs on a daily basis, which makes it easy for these doctors to gain access, and experiment. A 2005 survey found that between the years 1991 and 2001, roughly 80 percent of U.S. anesthesiology residency programs experienced problems with residents being impaired. Of those residency programs, 19 percent reported at least one death related to drug abuse.
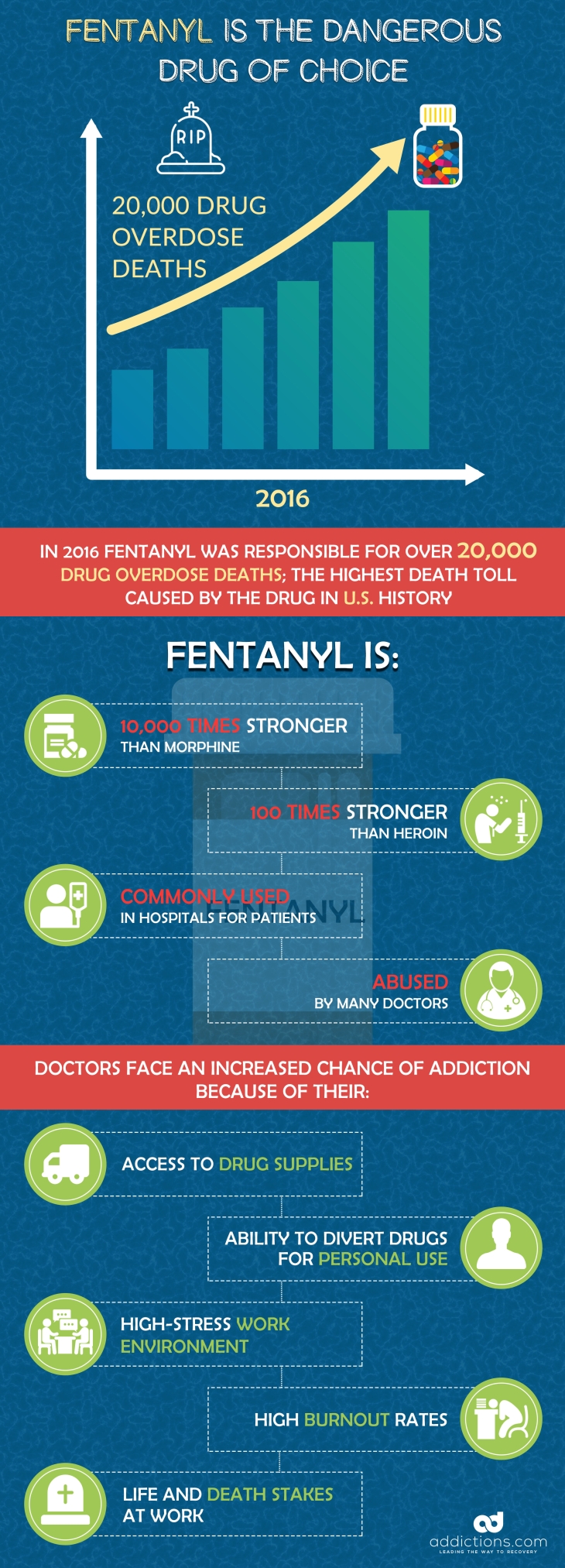
Why are these doctors becoming addicted to drugs? Studies show that anesthesiologists are often more susceptible to drug use disorders on behalf of the following factors.
Easy Access to Addictive Drugs
Anesthesiologists are in charge of administering and managing anesthesia that is given to patients during surgery and for pain management. These doctors have access to nearly every type of drug in large quantities, at any given time. Having easy access to highly addictive drugs often increases one’s risk for drug abuse and addiction — especially in anesthesiologists who work with these substances every day.
Ability to Divert Drugs for Personal Use
Some anesthesiologists who suffer from drug use disorders administer just a portion of drugs to their patients, and save the rest for themselves. For instance, doctors treating patients for pain relief may administer a portion of the dosage using a syringe, then hide the syringe and use it later to provide themselves with the remainder of the dose. This practice not only deprives patients of the necessary amount of pain relief, but can put both doctors and patients at risk for serious life-threatening diseases including AIDS and hepatitis C.
Spending Time in High-Stress Environments
Anesthesiologists spend lots of time in high-stress environments such as surgery rooms, emergency rooms, and intensive care units. Many doctors and nurses also work long shifts and get little sleep, and suffer burnout, physical stress, and mental stress as a result. Healthcare workers and those who suffer from substance use disorders in general often use alcohol and drugs to cope with stress.
Anesthesiologists: First Victims of the Opioid Crisis?
The U.S. opioid epidemic originated mainly on behalf of the overprescribing of painkillers, and painkiller abuse. Painkillers like oxycodone, hydrocodone, and morphine are highly addictive, and can quickly lead to tolerance and physical dependence when misused. Though opioid abuse generally starts at home with patients, family, and friends who have access to prescription painkillers, many tend to overlook the fact that anesthesiologists have greater access to an even larger supply of opioids.
Professors in the anesthesia and psychology fields say that anesthesiologists are among those who first started misusing opioids after they became more widely available. Opioids like morphine and fentanyl were originally developed for medical uses, but are now also used for recreation. Experts say that anesthesiologists were the first to begin using opioids for recreational use, since they had greater access to those drugs and could easily experiment.
Prescription opioid use became more nationally widespread during the 1990s, when pharmaceutical companies began to aggressively market oxycodone. Over the years, anesthesiologists have gained greater access to highly potent short-acting opioids like fentanyl. Fentanyl is currently one of the most deadly drugs in America, and continues to drive opioid overdose rates year after year.
Fentanyl Abuse Among Anesthesiologists On the Rise
Fentanyl is up to 10,000 times stronger than morphine, and up to 100 times stronger than heroin. In 2016, fentanyl was responsible for over 20,000 drug overdose deaths in the U.S. — the highest death toll yet caused by fentanyl. Fentanyl is now the number one drug of abuse among anesthesiologists, followed by sufentanil, meperidine, and morphine.
Studies reveal that the majority of anesthesiologists who die from drug-related deaths do so within their first five years of graduating medical school. Addiction among anesthesiologists is presumed to begin in medical school with the stages of initial use and experimentation. Experimentation can eventually turn into regular use, followed by tolerance, dependence, and lastly, addiction.
One study in particular shows that roughly 62 percent of U.S. medical school programs that specialize in anesthesiology have at least one student who suffers a drug use disorder. Among students that suffer drug use disorders, over 10 percent favor opioid tablets, while a staggering 64 percent favor fentanyl in the form of injections and patches.
Dangers Associated with Fentanyl Use Among Anesthesiologists
Increased fentanyl use among anesthesiologists is leading to a wide range of serious complications in hospitals, where patients are being directly affected by their doctor’s addiction. Many anesthesiologists with drug use disorders divert drugs from patients using syringes and needles — putting both themselves and their patients at risk for diseases including HIV, AIDS, and hepatitis C. Research shows that 41 percent of anesthesiologists who suffer drug use disorders prefer to use drugs intravenously.
Anesthesiologists who divert drugs from patients are also putting their patients at risk for tolerance, dependence, and unintentional overdoses. When doctors abuse their patient’s medication, other attending physicians can form the impression the dose isn’t working, and increase the patient’s dose — unaware that the anesthesiologist is using a portion of the drugs for themselves. Increasing a patient’s dose of fentanyl when they’re not truly tolerant to the medication can instantly lead to an overdose, or death.
The effects of fentanyl can also cause doctors to make serious mistakes while on the clock and attending to patients. For instance, an anesthesiologist under the influence of fentanyl can miscalculate a patient’s dose of potent drugs like morphine, and administer too little or too much — compromising their pain management or increasing the risk for an overdose. The sedative, drowsy effects of fentanyl can also prevent anesthesiologists from waking up from drug-induced slumbers when their assistance is needed in an emergency.
Anesthesiologists who suffer fentanyl abuse can safely recover at addiction treatment centers that have programs designed especially for this medical specialty. But despite fentanyl abuse being a rising problem, many anesthesiologists tend to avoid seeking addiction treatment on behalf of stigma.
Removing the Stigma Surrounding Doctors and Drug Use Disorders
Though addiction is widely recognized as a legitimate, chronic brain disease, this health condition continues to have a stigma. This stigma is made even worse when it comes to doctors and anesthesiologists who can potentially harm their patients and put lives at risk. A doctor addicted to drugs may be afraid they’ll lose their jobs or medical practices, or get them into serious trouble with the law if they admit to struggling with addiction.
Plus, stealing and diverting drugs from patients is considered an unethical medical practice, which can cause some doctors to experience psychological effects of depression and anxiety — further fueling their drug use disorder. Experts say factors such as these are what commonly prevent anesthesiologists from seeking help in the form of addiction treatment. This barrier also makes it difficult for researchers to determine the exact number of anesthesiologists suffering from addiction — indicating addiction rates could be far higher than initially suspected.
In addition to having to deal with the stigma surrounding doctors and drug use disorders, doctors who decide to seek addiction treatment must face controversy surrounding whether they should be allowed to return to operating rooms following rehab. Many argue that anesthesiologists should choose different medical specialties after having overcome addiction, despite the strict monitoring that would be in place when these doctors returned to work. Others argue that a case-by-case basis approach be used to determine whether certain individuals should be allowed to return to work as anesthesiologists.
A study examining chemical dependency among anesthesiologists found that most of these doctors can safely return to work as long as certain safeguards are in place to prevent these individuals from relapsing on the job. Safeguards used to protect these anesthesiologists include early detection, workplace drug testing, and referral to physician health programs responsible for managing and monitoring physicians who suffer drug use disorders.
Seeking Addiction Treatment as an Anesthesiologist
Anesthesiologists or other doctors who suffer from fentanyl abuse or substance use disorders often require specialized, intensive addiction treatment geared toward professionals in the medical field. Since their entire medical specialty revolves around administering drugs, anesthesiologists must learn the skills needed to work alongside these substances regularly without relapsing.
Here’s how fentanyl addiction is commonly treated among anesthesiologists and other doctors.
Treating Fentanyl Dependence
Fentanyl detox is the first stage of addiction treatment, and helps patients overcome physical dependence on this highly potent drug. Since fentanyl is short-acting and powerful, withdrawal symptoms normally begin within several hours of quitting use. Fentanyl withdrawal symptoms are often severe, and include diarrhea, increased heart rate, and vomiting.
Many addiction treatment centers use medication-assisted treatment, or MAT to help patients detox from fentanyl comfortably without suffering cravings and other symptoms. MAT involves the use of medications that reduce fentanyl withdrawal symptoms, and that block the effects of other opioids. Patients who use these medications can recover from fentanyl addiction while going about their daily lives, and avoiding discomfort associated with fentanyl withdrawal.
Buprenorphine, naltrexone, and methadone are commonly used in MAT to treat fentanyl dependence. Buprenorphine and naltrexone are used more frequently than methadone, since these medications are linked to higher treatment success rates and can even be used at home. Methadone-maintenance therapy, or MMT is only administered to patients at clinics to reduce the risk for abuse. Those who take part in MMT must visit methadone clinics or addiction treatment centers daily to obtain their daily dose of methadone.
Treating Psychological Causes of Addiction
After completing fentanyl detox, patients undergo a series of psychological therapies that address the underlying causes of their addiction. For anesthesiologists, this often involves 12-step support group therapy, relapse prevention training, and individual and group therapy aimed at professionals.
Most addiction treatment centers will customize therapies for patients based on their unique reasons for becoming a victim of fentanyl abuse. For instance, anesthesiologists who abuse fentanyl to cope with chronic stress will learn new, healthier ways to manage stress that don’t involve drug use. These doctors will learn that instead of turning to drugs to relieve stress on their lunch break, they can go for walks around the building for exercise, or use deep breathing techniques to relax naturally.
Ongoing care, also known as aftercare or continuing care, is crucial for helping anesthesiologists stay clean and avoid relapse after completing addiction treatment. Since overcoming addiction is often a lifelong journey, anesthesiologists need ongoing support to avoid resuming drug use — especially when surrounded by drugs and triggers at their jobs. When researching their treatment options, anesthesiologists should choose among rehab facilities that can take these special factors into consideration.